Published online: 3/31/2023
Access to emergency and essential surgical services is an important element of an effective healthcare system. The attention given to global surgery has recently increased, and initiatives like the World Health Organization’s Resolution 68.15 have called on countries to make progress in providing safe surgical care. As a surgeon who lived and worked in a remote area without electricity and most surgical resources, and now as an Ethiopian state minister, I am aware of the significant burden placed on individuals and families due to a lack of access to surgical services in low-resource settings, and I am excited to be a part of the development of innovative solutions to address this problem. Hopefully, my story will support and inspire clinicians, researchers, leaders, and governmental and non-governmental organizations across Ethiopia and throughout the world, working to ensure equitable access to and quality surgical services for all.
I was born and grew up in a small village in the rural part of Ethiopia, where access to good healthcare services was a distant dream for many people. I had the chance to witness countless deaths just due to a lack of access to essential health care, particularly emergency and essential surgical services. I shared the pain, lived with it, and lost many of my relatives and community members because of it. In this environment, I was inspired to pursue a career in medicine and eventually became a surgeon, determined to make a difference for the people of my home village.
After finishing high school and two years of preparatory school in that poor village, I was fortunate enough to join one of the universities in the capital of Ethiopia, Addis Ababa University, which was an opportunity I never thought was possible at the time. During my internship at the medical school, every time a uterine rupture presented, the patients mostly came from rural areas after being referred, and upon their arrival, they were exhausted; some of them died on the roads. Amusingly, these patients were mostly from my village, Merhabete, where I was born and raised. This made me feel a profound connection to the suffering of these people, and I felt a strong sense of duty to help them in any way I could.
Figure 2: Patient being carried to a health facility, where there are no roads or vehicles available.
After graduating from university, I returned to the rural villages, whilst I could have been assigned to the capital city with better medical facilities and higher salaries, I chose to work in the rural villages, not just to provide better healthcare and improve access but also because I saw how much of a difference I could make. During this time, I began to understand the system challenges of providing surgical services in low-resource settings.
The first challenge was a lack of human resources, as the village had no general surgery, obstetrics, or anesthesia specialists, and I was only a general practitioner. As part of the solution, my nurse colleague and I took a three-month course in emergency anesthesia and surgery, respectively, and returned to work. These enabled us to perform emergency CS, hysterectomy, appendectomy, bowel resection, anastomosis, and trauma-related procedures, which are now called the Bellwether Procedures. At least pregnant women and people with severe injuries were spared having to travel 180 km by gravel road across deserts and steep cliffs to a nearby hospital, which would further complicate their situation.
The second challenge was te cultural norm of the community not visiting the health care facility early for medical care, often waiting too long to seek treatment. This was especially difficult for mothers who were forced to give birth at home with traditional birth attendants and considered going to the hospital a taboo, which resulted in life-threatening complications and came to the health facility when it was often too late. To combat these issues, the hospital staff worked diligently to develop a strong rapport with the local community by organizing education campaigns and programs. We also invited mothers treated at our facility to participate in promotional activities, and we met with birth attendants to address their concerns and ensure they referred mothers in need of medical attention earlier. All these efforts have increased the number of patients admitted to our hospital.
Figure 4: Alem Ketema Hospital, North Shewa, Amhara region, Ethiopia
Despite the assistance we were receiving from the Menschen for Menschen program established by Dr Karl Heinz Boem, who was constantly donating and supporting this hospital with equipment, beginning with upgrading, and furnishing our hospital from a small health center, other challenges included insufficient funding and staffing levels, as well as a limited supply of some surgical equipment and blood products. We began contacting the Ministry of Health and regional health bureaus to address these issues while also attempting to use all preventive and treatment measures to help our patients with our limited resources. In such a situation, I worked for three years as an emergency officer and then I left the village to advance my education by specializing in obstetrics and gynecology.
Following my specialty training, I returned to this community, and most challenges remained unresolved, and some had even worsened, though the community’s needs are increasing. People needing surgery could not be accommodated, so a substantial number of those cases were referred to the nearest hospital, located more than four hours away, where they also might be told to come back after a week or months. Often, I am asked to operate on brain tumors, which is not my area of expertise, because people think you can operate on anything if you open up an abdomen. This is the point at which I realized that I had to look beyond providing medical care and toward leadership to make a meaningful and lasting impact on these people’s lives that is not dependent on individual efforts.
After working in these circumstances for four years while being highly involved in the hospital’s leadership and approaching the ministry with ideas and proposals to improve the quality of care, I was able to see the impact of my and my team’s hard work and dedication on the community. Today, for the same catchment population, there are three more hospitals than one, 20 more health centers, and 84 more health posts in that district and the surrounding area. There are two obstetricians, four general surgeons, and more than 10 operating tables. The number of general practitioners and other professionals involved in surgical and overall healthcare delivery has grown more than fivefold. Healthcare budget allocations from the regional bureau and ministry as well as other investments have increased significantly. With all these resources, we expect to have bridged the three delays related to poor access and healthcare quality. All of these achievements make me smile, and indeed, these small achievements should be celebrated as they give energy for bigger things to come.
After the four years, I moved to Addis Ababa, the capital, and became the chief clinical director of the government hospital. In 2022, I ran for a political office at the federal government, representing my small village there, and now I am a member of the parliament and state minister of Ethiopia’s ministry of health. Through all these experiences, I have learned precious lessons and understood that unless a change has been made to the overall health system and leadership, the challenges, whether in rural or urban areas, will remain a hindrance to the development and progress of Ethiopia.
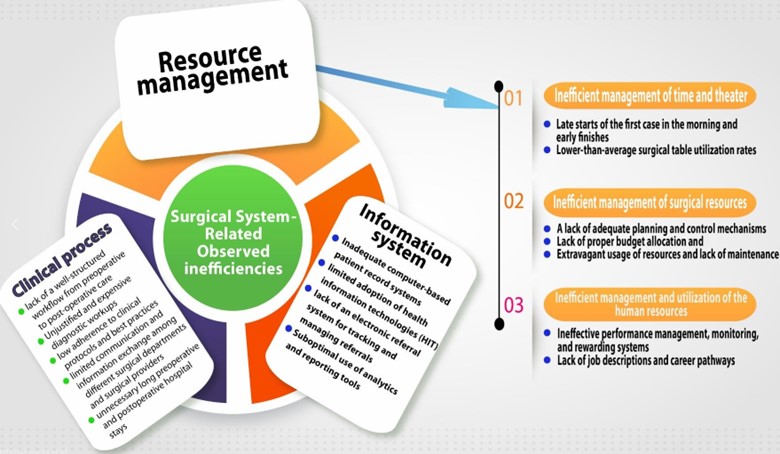
Even though much progress has been made in Ethiopia in improving surgical access in the past few years, only 300,000 surgeries are performed each year, while many people need surgeries. Several system-related inefficiencies continue to hinder our performance, which as per my observation I can classify them into three categories: resource management, clinical processes, and information systems. Several factors contribute to inefficient resource management, including inefficient use of operating rooms and operating time because of long workflow processes, resulting in late starts and early finishes, and even elective surgery is not performed in most of our referral hospitals in the afternoon: and lower-than-average surgical table utilisation rates. Plus, a lack of adequate planning and control mechanisms, extravagant usage of resources, and proper budget allocation also contribute to the inefficient management of surgical resources. Inadequate surgical equipment and maintenance result in recurring supply shortages, including anesthesia drug shortages, operation delays, and cancellations.
Furthermore, ineffective performance management, monitoring, and rewarding systems, a lack of job descriptions and career pathways, and a lack of an accountable culture all contribute to inefficient management and utilization of the human resources that are at hand. Due to these and the other reasons mentioned, surgical workforce productivity is low, even in most of our big referral facilities: the number of surgical procedures per surgeon per month is less than 12.
Clinical process inefficiencies include the following: Unjustified and expensive diagnostic workups result in a high cancellation rate—as high as 35% in some specialized hospitals—low adherence to clinical protocols and best practices, limited communication and information exchange among different surgical departments, hierarchical barriers limiting the potential for open dialogue and discussion among care providers, and unnecessary long preoperative and postoperative hospital stays. Inefficiencies in clinical processes result in extended stays for patients and lower quality of care.
Finally, information systems inefficiencies include inadequate computer-based patient record systems, limited adoption of health information technologies (HIT), a lack of an electronic referral system for tracking and managing referrals, and suboptimal use of analytics and reporting tools. All these results in limited monitoring of performance indicators and limited evidence-based decision-making due to the need for a comprehensive data collection system.
Figure 6: Summary of the observed surgical-related inefficiencies
As a result, I believe it is time to reconsider our care coordination and integration models in Ethiopia and Africa in general, as the problems are mostly the same: improving care continuity and collaboration through data-driven decision-making, institutionalizing a culture of continuous improvement, occasionally enforcing accountability, and rewarding excellent behavior. For an efficient, accessible, and safe surgical service, person-focused and population-based care through vertical and horizontal integration are highly needed. Such integration requires micro-level clinical integration, such as standardizing clinical processes and protocols, optimizing resource utilization, and providing access to health information systems , meso-level professional and organizational integration, such as training medical and nursing staff on quality assurance, effective use of health information technology; and macro-level integration such as intersectoral collaboration, as well as macro-level policy coordination and strategic system integration. Furthermore, functional, and normative integration can ensure system connectivity at all levels, and it is critical to establish public-private partnerships to facilitate collaboration and knowledge transfer as well as to maximize resources.
In conclusion, the experience i had working in that small rural – village, then as a hospital director in the capital, and now as a minister in the Ministry of Health of Ethiopia has given me a basic understanding of the inefficiencies that are a bottleneck to providing a sustainable, safe, and efficient surgical service as well as for improving the system. In my capacity as someone who understands global surgery concepts and the importance of sharing experiences and learning, I believe that sharing this story will be beneficial to many of my colleagues as well as public and private institutions that are working to improve surgical care in Ethiopia and other low-income countries, since many of the challenges faced are likely to be similar.
Thus, integration is essential for the effective and efficient functioning of a healthcare system, with micro-level clinical integration aiming to standardize processes and protocols, optimize resource utilization, and improve the health information systems; meso-level professional and organizational integration striving for enhanced collaboration between healthcare professionals and organizations; and macro-level political integration to create a more conducive policy environment in terms of financial support, quality assurance, and public engagement.
All of these are essential for improving the surgical system in LMICs, and this has to be led by more collaborative, evidence based decision making in order to ensure better patient outcomes and ultimately contribute towards achieving Universal Health Coverage (UHC).
Author: Dr. Ayele Teshome
State Minister
Ministry of Health, Ethiopia.
email: - ayele.teshome@moh.gov.et
Acknowledgement
F.Kifle assisted with the writing of this article.
Subscribe to our newsletters to receive such great stories and stay up-to-date with the latest news and trends in your inbox. Don’t miss out on exclusive offers and promotions! Click Here >
Do you want to share your story with us in our upcoming issue?
Contact us
Tell: +251 919 118 715
Office Tell: +251 111 542 454
Email: blogs@old.n4pcc.com, info@old.n4pcc.com
Office: Addis Ababa, International Leadership Institute, Office Number 111